What Is COVID-19?
What Is COVID-19?
This story is part 3 of a series. If this is your first time reading, you may want to read Part 1: What Is A Virus, and Part 2: What Is SARS-CoV-2? first. This will give you a general understanding of what a virus is and some more specific understanding of the Novel Coronavirus SARS-CoV-2.
In 2019 a cluster of people in China became sick with pneumonia. As medical professionals began to investigate the disease, they discovered that it had been caused by a “Novel” virus – one that is new to medicine or that has not been seen before. This virus was given the name 2019-N-CoV, and is now called SARS-CoV-2.
As doctors began to investigate, they found that all of the patients could be traced back to a seafood and live animal market in the city of Wuhan, China. From the market, it soon spread to friends and family members, as well as the medical professionals who treated them.
One of the doctors involved in treating those early patients, Li Wenliang, also contracted the virus and became sick with the disease. On December 30th, 2019 he sent a warning to his fellow medical professionals. His work with COVID-19 began when he observed that the cases and symptoms reminded him of SARS – a disease that led to a global epidemic in 2003. He died of COVID-19 on February 7th at the age of 33.
Viruses cause disease when they get inside the cells of your body and hijack them, forcing the cells to replicate the virus and spreading the new copies throughout the rest of your body. The more cells that are infected to reproduce the virus, an exponential increase in the number of viral cells are created. This is the etymology of the term ‘going viral’ as we refer to it about ideas or on the internet or in social media.
When a virus, including SARS CoV-2, gets inside your body there is an “incubation period” – this is the period of time from the point when you first become infected with a disease to the point at which you begin to show symptoms. For COVID-19, the incubation period can be as long as 14 days. Some people begin to show symptoms as soon as 2 days after infection, but the median incubation period for COVID-19 is 4 to 5 days.
Some people who become infected will not feel sick and do not ever exhibit symptoms. These cases are called asymptomatic. If you are exposed to COVID-19 and eventually show symptoms, the period of time for which you were sick but were not showing symptoms is called presymptomatic. It is important to note that it appears that people can spread the virus even when they are asymptomatic or presymptomatic. Some estimates suggest that as many as 30% to 40% of cases of COVID-19 are asymptomatic. This is why it is so important that everyone follows the recommendations of public health authorities to prevent further spread – if someone chooses not to wear a mask or social distance because ‘they feel fine’ they could be spreading the disease to someone else in the community – potentially someone who is more susceptible to the disease and who may eventually die.
How It Spreads
SARS-CoV-2, the virus that causes COVID-19, spreads from an infected person to others through respiratory droplets and aerosols created when an infected person coughs, sneezes, sings, shouts, or talks. The droplets vary in size from large droplets that fall to the ground rapidly (within seconds or minutes) near the infected person, to smaller droplets, sometimes called aerosols, which linger in the air under some circumstances.
The relative infectiousness of droplets of different sizes is not clear. Infectious droplets or aerosols may come into direct contact with the mucous membranes of another person's nose, mouth or eyes, or they may be inhaled into their nose, mouth, airways and lungs. The virus may also spread when a person touches another person (i.e., a handshake) or a surface or an object (also referred to as a fomite) that has the virus on it, and then touches their mouth, nose or eyes with unwashed hands. – Canada.ca
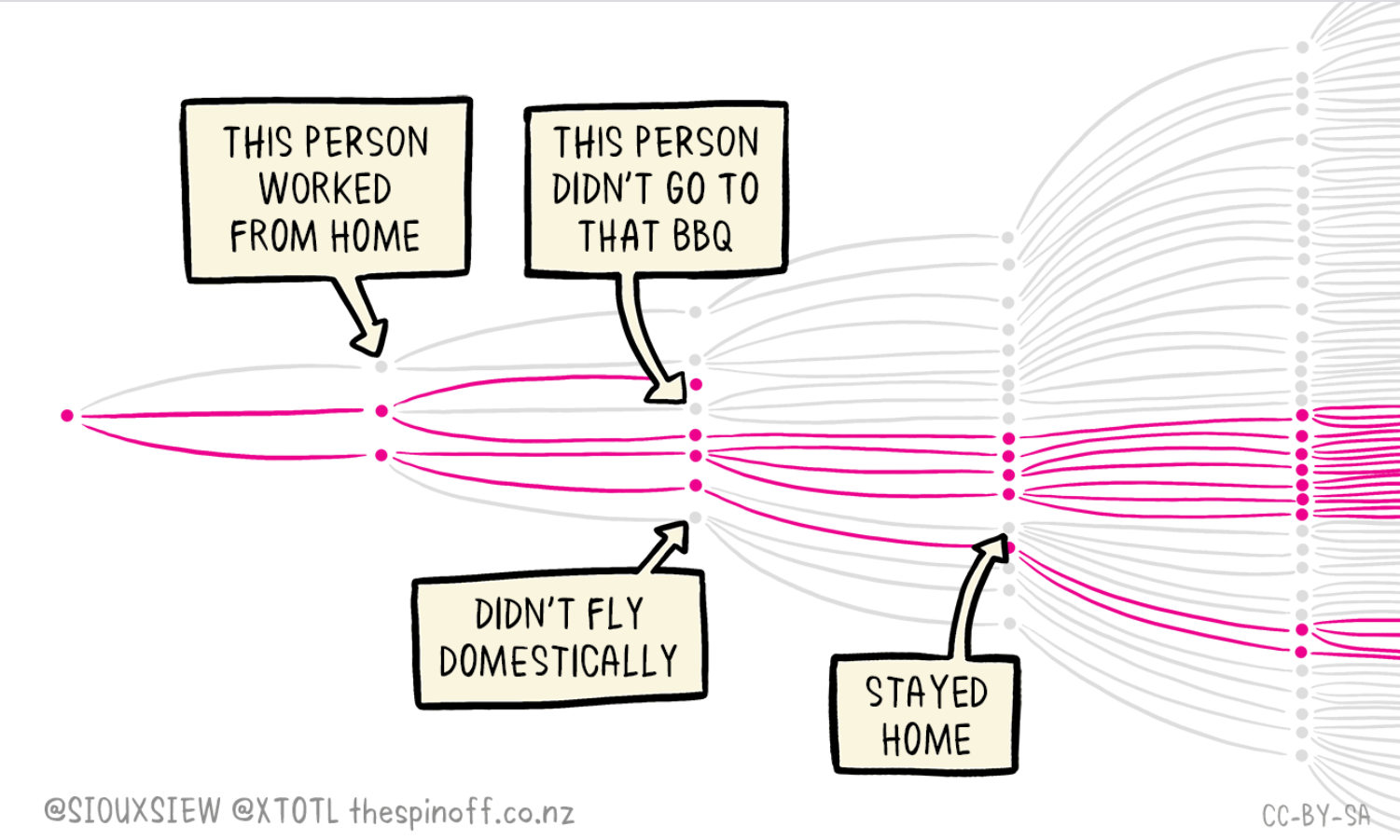
The SARS-CoV-2 virus has a high R0 ("R - naught”) – the number of additional people whom one person with the disease will infect. While it’s not yet known exactly what the R0 of SARS-CoV-2 is, many estimates place it around 2.5 That means that each person with COVID-19, on average, will give it to 2.5 other people.
For simplicity, let us assume that the R0 was only 2:
If 1 person infects 2 others, then those two new cases each infect two others leading to 4 cases, and those 4 each infect two more leading 8 cases. These numbers may seem small, but they are exponential. 2 becomes 4, then 8, 16, 32, 64, 128, 256, 512, 1024, 2048, 4096, 8192, 16384, 32768, 65536, 131072, 262144, 524288, and after twenty cycles: 1,048,576.
Yes, with a disease like COVID-19 one person who wears a mask at the grocery store when presymptomatic can prevent more than 1,000,000 other infections.
Compare this level of spread to that of the average seasonal flu with an R0 of approximately 1.27. After 20 cycles of spread 1 person with an infection rate of 1.27 leads to only 119 infections. 119 versus more than 1,000,000 – and that is why, regardless of the severity of the disease, the mortality rate, or any other factors, we all need to take responsibility for stopping the spread of COVID-19.
In Saskatchewan, the first presumptive case of COVID-19 was identified on March 12, 2020. From March 12th until November 4th (237 days) there were 3, 408 cases identified. In the subsequent 20 days (November 5th through November 24th) there were an additional 3,475 cases - more than a doubling of the number in a very short period.
Managing and taking precautions against COVID-19 isn’t only about you – it’s about everybody else around you. This is why governments and public health authorities mandate social distancing, staying home, and limit the size of groups. These precautions help protect you, but they aren’t designed specifically to protect YOU as an individual - they are designed to protect everyone else from you. If I protect YOU and you protect ME, then we protect each other, and that is how the pandemic comes to an end.
What The Disease Does
SARS-CoV-2 first infects the cells lining your throat, airways, and lungs. At this point you will not feel sick, but your body is rapidly producing copies of the virus. For many people, a mild sickness is all they will ever experience, and some percentage of those may not even know they are sick.
Common symptoms of COVID-19 include:
• New or worsening cough
• Fever
• Difficulty breathing
• Feeling tired
• Abdominal discomfort
• Click here for a full list of common symptoms
These symptoms are a result of your immune system fighting against the virus that is infecting your body. As the immune system reacts, it can trigger inflammation in the lungs – which is called pneumonia. As inflammation in the lungs become more severe, tiny sacs deep in the lungs called alveoli begin to fill up with water and can cause shortness of breath and difficulty breathing. As the sickness worsens, some people will no longer be able to get enough oxygen into their bloodstream through regular breathing. Doctors will need to put those patients on supplemental oxygen, and some of those people may eventually need to be intubated and placed on a ventilator.
However, in some people, the immune system will go into overdrive and begin attacking the body it is trying to protect. In the most severe cases, this can cause the kidneys to fail, preventing them from properly cleaning your blood, damaging the lining of your intestines, the heart, and more. It can also lead to permanent health problems including lung damage, heart damage, septic shock, kidney damage, liver damage., multiorgan failure, and more, including death.
In some rare situations children can develop a severe inflammatory syndrome a few weeks after infection.
According to the CDC, about 80% of the people who get COVID-19 recover from the disease without needing hospital treatment. About 20% of those who get COVID-19 will become seriously ill and require oxygen or other medical interventions, and 5% of people will become critically ill and need intensive care. As of November 25, 2020 the global death rate for COVID-19 was more than 1.4 million people.
Risk Factors For Severe Illness
The people who are most at risk of severe illness from COVID -19 include those aged 60 and older, those with other underlying medical problems such as high blood, pressure, diabetes, heart and lung infections, obesity, or cancer. However, anyone can get sick with COVID-19 and become seriously ill or die at any age.
Why It Matters
If 80% of the population will recover fine from the disease, then why is this such a big deal? Simply put, because 20% of the population won’t. Taking simple precautions can help us all protect 1 in 5 people from serious sickness and risk of death.
Medical systems are not designed to deal with mass outbreaks or mass emergencies; special considerations and plans must be put into place. With a disease such as COVID-19, which spreads very quickly, this can quickly lead to a medical system which is overwhelmed. As a disease spreads and cases rise an increasing percentage of the overall available medical resources needs to be applied to those who are sick with COVID-19 over other diseases. At some point, the medical system becomes so overwhelmed that elective procedures are delayed, treatments for other diseases such as cancer are pushed back, and even emergency medical attention from heart attacks and car accidents can be impacted. This can lead to further loss of life. Eventually, as happened in Italy, doctors may be forced to make decisions about which patients receive medical care, and which do not.
Canada is generally well-prepared for pandemics due to good planning and a high quality of health care. In addition, our nation gained a lot of experience during the SARS outbreak in 2003, where Toronto was an epicenter of the disease.
No one is truly safe, even the otherwise healthy, and we must all work together to protect each other.
Treatment Options
Because COVID-19 is caused by a virus, antibiotics do not help to treat the disease and should not be used for prevention or treatment.
Most people who become ill with COVID-19 will be able to recover at home. Some of the same things you do to feel better if you have the seasonal flu – getting enough rest, staying well hydrated, and taking medication to treat the symptoms will also help you recover from COVID-19.
As doctors and scientists learn more about SARS-CoV-2 and COVID-19, new drugs and treatments are being developed. The antiviral drug Remdesivir was approved by the CDC in October of 2020 to treat certain hospitalized patients with COVID-19. Sometimes a class of steroid called a cortisteroid is administered to patients who have a hyper-immune response to help counteract the immune system’s overreaction that is causing damage and often leads to the most severe symptoms, including death. These drugs are potent anti-inflammatories and are typically readily available and inexpensive.
Some drugs, such as Chloroquine or hydroxychloroquine received a lot of attention early in the pandemic. These drugs are typically used to treat malaria and other inflammatory diseases such as lupus and rheumatoid arthritis. However, subsequent studies have shown that this is inconclusive. The recommendations are that chloroquine or hydroxychloroquine should not be used to prevent or treat COVID-19 infections unless it is being prescribed in a hospital as part of a clinical trial.
There is currently no cure and no single drug that can be used to treat or prevent COVID-19. The best offense against COVID-19 is a good defense against becoming infected in the first place.
Prevention And Protection
This is the subject of the next phase in this series. In general, however, wash your hands regularly, wear a mask when going out in public, and limit your interactions with other people, forming a social bubble or ‘cohort’ to prevent the spread of the disease. Follow public health guidelines; they are there to protect you and keep you safe.
Stay up to date with information on the Government of Canada’s website
Read the Saskatchewan public health guidelines
Reinfections
In the case of some diseases, once you get the disease you have trained your immune system to fight a certain infection you are unlikely to get the disease again. Children born before the 1980s were often expected to get Chickenpox and were sometimes even sent to play with other kids who had Chickenpox in order to ‘get it out of the way’ and build immunity. In some rare cases this would lead to severe illness or death, and in some cases children could become reinfected a second time.
However, this is not he case with COVID-19. Already some people have become infected with COVID-19 a second time. As further testing and tracing is done, doctors will be better able to understand how prevalent reinfection might be. However, other coronaviruses are often able to reinfect people, with immunity lasting several months, but not indefinitely.
A bright spot in this research, however, is that subsequent infections do seem to be milder than the initial case, with the individual’s immune system understanding what to do. However, no one knows the long-term implications of this disease. Just as recovering from Chickenpox makes you susceptible to Shingles later in life, there may be complications down the road from COVID-19, even for those who recovered easily.
COVID Long-Haulers
With many illnesses, such as a cold or the flu, we are used to recovering from the disease and feeling better relatively soon. With COVID-19 there is an increasingly common trend being noticed: the long-haulers. COVID long-haulers are people who seem to have recovered from the disease, but continue to suffer lingering effects, including shortness of breath, fatigue, aches, and more.
While the likelihood of long-term effects is not known, it does not seem to be directly related to the severity of the original infection. As this article from SCIENCE states, there are people with mild symptoms who have long-term issues and people who had significant difficulties with COVID who seem to be fully recovered.
Debunking Coronavirus Myths
There is a lot of misinformation about COVID-19. In part, this is because there is a novel disease and as we began the pandemic people were eager to come up with solutions and explanations. Other pieces of misinformation may have been created to intentionally mislead the public.
The WHO has a comprehensive webpage debunking COVID-19 myths that you should read. Notably:
5G cell phone towers do NOT cause COVID-19. Viruses cannot travel over radio waves or mobile networks
Eating garlic will NOT prevent you from getting sick with COVID-19
Drinking bleach will not prevent or cure COVID-19 AND IS VERY DANGEROUS
People of all ages and health levels can get sick and die from COVID-19, not just the elderly
COVID-19 is not the same as the seasonal influenza or a common cold
Additional Resources
CBC Saskatchewan - Faces of COVID-19
Did you find this helpful? Consider making a donation to the Saskatchewan Science Centre!